
Dequacia Catlin is a nursing student in her senior year at Lincoln University. In 2022, she received an email from the university inviting her to apply for an internship with Americorps’ Public Health Nursing Fellowship. She was selected and placed at ChesPenn’s Center for Family Health at Coatesville in October.
Dequacia remembers that her interest in nursing goes back 10 years. “When I started in community college I majored in criminal justice, but it didn’t feel like my niche. In 2012 I took a Certified Nursing Assistant (CNA) course and when we had our clinicals I liked it. I started working at the hospital as a CNA.” Later she went on to enroll in Lincoln University’s Bachelors program in nursing.
“In the beginning my academic experience was a little tough. You start with the prerequisites and then you’re thrown into this program where you are required to critically think. But as I learned and did some tutoring, my grades got better.” Her grades were critical to her success. Lincoln requires a B average to remain in the nursing program. She shared that, “ I’ve been on the Dean’s List every semester. I’ve been really grateful to Lincoln University because they push their students.” They push us to learn clinical reasoning and judgement.” She’s also enjoyed the friendship and support of the staff. “ChesPenn has been really great to me. I’ve learned things. I really like it. I can learn here.”

Dequacia has encountered surprises and some challenges along the way. She’s learned a lot about what it means to provide care in a vulnerable community. “Some things have surprised me as far as interacting with the patients. Just seeing the diverse community that comes here – no matter who they are or whether they speak English or not we’re able to communicate with them and give them the best care possible. I really love that ChesPenn is able to relate to the patients. They really trust the staff – the front desk staff are so open. That makes a difference in a person’s life. I feel that ChesPenn goes beyond to make the patient feel like a person. In other places I’ve seen the patient is more like a number, but here, they know their name, their children, their family.” She also acknowledged the challenge of contacting patients who often rely on prepaid phones or who may take time to get back to us.
An avid traveler, Dequacia has visited countries in Latin America and the Caribbean and has studied in Ghana. In her travels, she’s seen the impact of health disparities in in the regions she has visited. Her experience has inspired her ambition to pursue a career in public health. And she has very specific goals – first, to work at the county level in health and human services while she works on a master’s degree in public health, then a role at the CDC and on to the World Health Organization.
Even Dequacia’s leisure time is dedicated to community service. She belongs to Chi Eta Phi Nursing Sorority. When she’s not in school she often volunteers in the community.
ChesPenn nurse Kenisha Parks has served as Dequacia’s mentor at ChesPenn. She has been impressed with the Americorps nurse internship program and especially with Dequacia. “You don’t run across those kind of students all the time” she commented. “ The patient comes first with her always. She’s going to go a long way.” We’re proud to be part of her journey.

 Alex Kocsik can’t remember the exact moment she decided on a career in healthcare, but by age 13 she knew she would become a doctor. She volunteered as a Candy Striper in high school and simply continued her career path from there. She liked the stepwise trajectory from college to medical school to residency. It gave her a clear goal to work toward at each stage of her education.
Alex Kocsik can’t remember the exact moment she decided on a career in healthcare, but by age 13 she knew she would become a doctor. She volunteered as a Candy Striper in high school and simply continued her career path from there. She liked the stepwise trajectory from college to medical school to residency. It gave her a clear goal to work toward at each stage of her education.


 Open enrollment for insurance through the Health Insurance Marketplace® begins November 1 and continues through January 15, 2023. During this time, you can enroll in, re-enroll in, or change a 2023 health plan through the Health Insurance Marketplace®. Coverage can start as soon as January 1, 2023.
Open enrollment for insurance through the Health Insurance Marketplace® begins November 1 and continues through January 15, 2023. During this time, you can enroll in, re-enroll in, or change a 2023 health plan through the Health Insurance Marketplace®. Coverage can start as soon as January 1, 2023.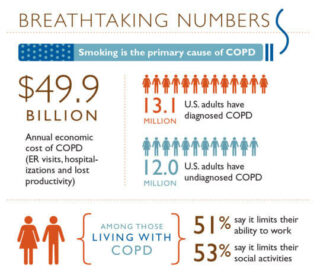 November is COPD Awareness Month – and not coincidentally, The Great American Smokeout is on November 17. COPD, or chronic obstructive pulmonary disease, is an umbrella term for emphysema and chronic bronchitis. Smoking is its primary cause.
November is COPD Awareness Month – and not coincidentally, The Great American Smokeout is on November 17. COPD, or chronic obstructive pulmonary disease, is an umbrella term for emphysema and chronic bronchitis. Smoking is its primary cause.




 Chelsea Spiegelhalder’s family has deep roots in Coatesville. Her grandmother was a nurse at Coatesville Hospital long before it became Brandywine Hospital. Her father was a pharmacist. All of her family members have volunteered in local organizations and in their church. Chelsea herself has served on the Board of Directors of a local nonprofit. Many of her patients know her or her family because of their work in the community. That relationship often makes it easier for patients to trust Chelsea’s advice about managing their health.
Chelsea Spiegelhalder’s family has deep roots in Coatesville. Her grandmother was a nurse at Coatesville Hospital long before it became Brandywine Hospital. Her father was a pharmacist. All of her family members have volunteered in local organizations and in their church. Chelsea herself has served on the Board of Directors of a local nonprofit. Many of her patients know her or her family because of their work in the community. That relationship often makes it easier for patients to trust Chelsea’s advice about managing their health. Every October, pink ribbons appear all around us – on social media, in the news, even on food items. Breast Cancer Awareness Month will be on many minds this month, so it’s a great time to answer some common questions about what may put you at risk and what may help protect you:
Every October, pink ribbons appear all around us – on social media, in the news, even on food items. Breast Cancer Awareness Month will be on many minds this month, so it’s a great time to answer some common questions about what may put you at risk and what may help protect you:



